The Patient Journey
Imagine you have to give yourself an injection… right this instant!
If you have never done this before, chances are you will find yourself in an extremely anxious state. “How bad will this hurt?” “Will I find the right spot?” “Can I finish the job without panicking or making a mistake?” Don’t forget… right now you feel physically ill and emotionally distressed. Focusing on ANYTHING is HARD.

Flash forward six months. You hold a completely different set of attitudes. You are feeling better, and you’ve become an injection pro… you’ve injected yourself close to 400 times now! There’s nothing scary about it. It’s actually somewhat of a nuisance now. The device takes too long to use…requires too many steps. It’s not very convenient either…it needs to be smaller, and easier to take on-the-go. You even consider certain aspects of its design as ridiculous, and clearly not designed with you in mind. You are often annoyed with the delivery system and the therapy you feel trapped within. You seriously consider skipping a dose on occasion…maybe you already have.
One Patient…Many Users
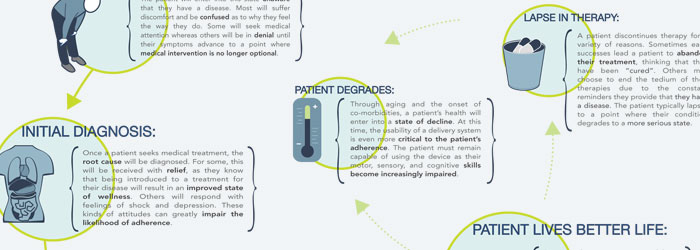
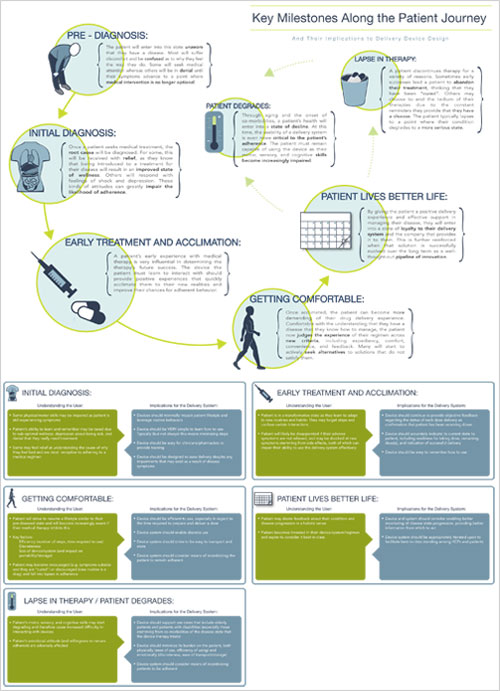
We all probably recognize that no two patients are completely alike, but how many of us ever consider how no ONE patient is alike when viewed over time. A patient’s progress through disease management is a Journey where they migrate through different stages that affect the way they think and the things they are capable of. This has implications for how a delivery system, through the way it is designed, needs to support them, and influences the very meaning of what “usability” is. To better understand this concept, we can focus on two very different points on the Patient Journey timeline that serve as examples of the just how different the use cases that delivery devices need support can be.
The Struggle to Adapt and Learn

Early on, patients who use delivery systems as a component of their medical therapy are struggling to cope with some very significant life disruptions. Most likely, they are not feeling very well in a physical sense. Emotionally, they are likely fluctuating between fear, anger, and deep concern or depression. And now they are being asked to take on new responsibilities, learn new tasks, and quickly become experts in managing parts of their disease.
What does this mean for a device? We need to qualify ease of use further by ensuring that device operation requires as few steps as possible in order to best assure that users can learn, remember, and quickly master its use. And devices need to provide clear and absolute confirmation that they were used properly and delivered the medicine successfully. Ambiguity relative to delivery serves to heighten patient anxiety, can lead to overdosing, and can cloud perceptions that the device is trustworthy or effective which in turn compromise adherence.
This also means that ease of use should translate into “easily demonstrable”, as patients will likely be reliant on the support of HCPs and family members to help them learn about and operate the device as they cope and acclimate themselves. Optimizing designs for both self administration as well as demonstration need to carefully consider how we as humans learn, and the differences between how we process information by watching others versus doing ourselves. Failing to support these early stage requirements can lead patients to quickly abandon therapies.
Staying Faithful

Later stages may see patients returning to a more stable condition and reasonable quality of life. Device use has probably been mastered, and now the patient becomes more demanding regarding how the device supports, or in many cases doesn’t support, quality of life. Subsiding anxieties make room for motivations based on convenience, or confidence that “I have this disease beat…at least for today.” As patients settle into this “new normal”, these attitudes can lead to skipped doses and lapses in adherence, often throttling the patient back to a state where the disease manifests itself more seriously.
In this state, a delivery system still needs to support efficiency and minimal steps, but now for different reasons based on convenience and lifestyle enhancement. Feedback also needs to be considered differently, and should strive to incentivize patients to remain adherent in order to maintain control of their disease and even, where possible, improve upon their condition.
The Big Lesson
There are many other points along the Patient Journey, but by realizing this idea alone, device manufacturers can better understand the complexities behind exactly what user-centered design really means. Armed with this awareness, we are better enabled to design and develop safe, reliable, and desirable solutions that address the shifting nature of what usability means for all the types of patient that one patient might be.
To receive a full size hi-resolution poster, or for more information on this topic, please email Mark Tunkel, Partner and Director of Business Development, at mtunkel@insightpd.com
