One Patient, Many Users
While we all likely recognize that no two patients are completely alike, what many of us never consider is that no individual patient is alike when viewed over time. A patient’s progress through disease management and the emotional stages of chronic disease is a very involved journey that impacts the way they think and what they’re capable of. This has implications for how a delivery system’s design needs to support patients, and influences the very definition of “usability” in real time.
Over the course of the past several years, we’ve conducted numerous research studies to explore patient needs and discovered that a clear understanding of key patient milestones and emotional stages of chronic disease can afford pharma companies significant opportunities to differentiate themselves through transformative innovation.
A thorough understanding of user and clinical stakeholder needs allows developers to characterize and prioritize them across multiple dimensions to help proactively make decisions regarding the definition of drug delivery offerings that might include novel development or selection of platform delivery devices, strategies for training and onboarding, as well as supporting longitudinal adherence through companion software and device connectivity.
Two of these studies include The Patient Journey, and Attitudinal Archetypes of Chronic Disease Management.
The Patient Journey
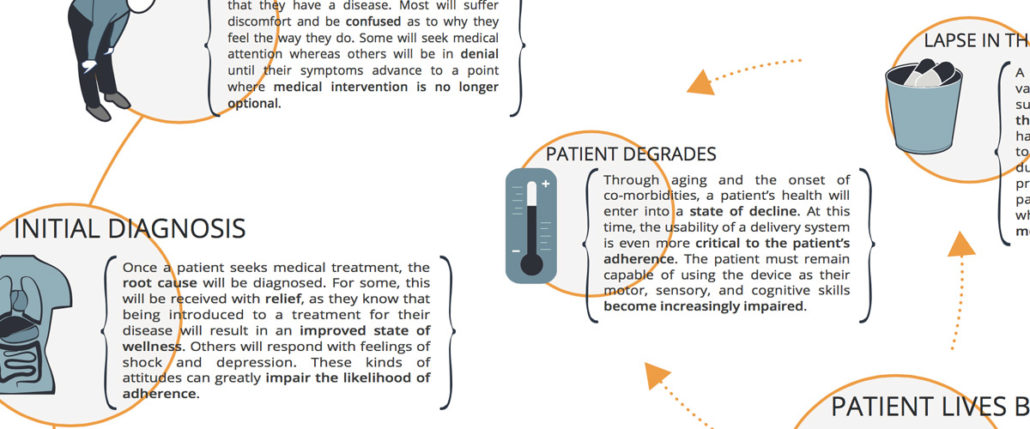
Key Milestones
Imagine you have to give yourself an injection – this instant! If you’ve never done this before, chances are you will find yourself in an extremely anxious state. “How bad will this hurt?” “Will I find the right spot?” “Can I finish the job without panicking or making a mistake?” Don’t forget, right now you feel physically ill and emotionally distressed. Focusing on ANYTHING is HARD.
Flash forward six months. You hold a completely different set of attitudes. You are feeling better, you’ve become an injection pro, and you’ve injected yourself close to 400 times now. There’s nothing scary about it. It’s actually somewhat of a nuisance now. The device takes too long to use, requires too many steps. It’s not very convenient either. It needs to be smaller, and easier to take on-the-go. You even consider certain aspects of its design to be ridiculous, and clearly not designed with you in mind. You are often annoyed with the delivery system and the therapy you feel trapped within. You seriously consider skipping a dose on occasion. Maybe you already have.
Key milestones along the Patient Journey include pre-diagnosis, initial diagnosis, early treatment and acclimation, and for some, mastery. Within these milestones, a myriad of variable needs and opportunities exist for delivery device platform innovation. To better understand this concept, we can focus on two very different points on the Patient Journey that serve as examples of just how different individual patient needs for their delivery devices can be.
The Struggle to Adapt and Learn
Early on within the context of early treatment and acclimation, patients who use delivery systems as a component of their medical therapy are struggling to cope with some very significant life disruptions. Most likely, they are not feeling very well in a physical sense. Emotionally, they are likely fluctuating between fear, anger, and deep concern or depression. And now they are being asked to take on new responsibilities, learn new tasks, and quickly become experts in managing parts of their disease.
What does this mean for a device? We need to qualify ease of use further by ensuring that device operation requires as few steps as possible in order to best assure that users can learn, remember, and quickly master its use. And devices need to provide clear and absolute confirmation that they were used properly and delivered the medicine successfully. Ambiguity relative to delivery serves to heighten patient anxiety, can lead to overdosing, and can cloud perceptions that the device is trustworthy or effective which in turn compromise adherence.
This also means that ease of use should translate into “easily demonstrable”, as patients will likely be reliant on the support of healthcare providers and family members to help them learn about and operate the device as they cope and acclimate themselves. Optimizing designs for both self-administration as well as demonstration need to carefully consider how we as humans learn, and the differences between how we process information by watching others versus doing ourselves. Failing to support these early stage requirements can lead patients to quickly abandon therapies.
Staying Faithful
Later stages along the Patient Journey may see patients returning to a more stable condition and reasonable quality of life. Device use has probably been mastered, and now the patient becomes more demanding regarding how the device supports, or in many cases doesn’t support, quality of life. Subsiding anxieties make room for motivations based on convenience, or confidence that “I have this disease beat…at least for today.”As patients settle into this “new normal”, these attitudes can lead to skipped doses and lapses in adherence, often throttling the patient back to a state where the disease manifests itself more seriously.
In this state, a delivery system still needs to support efficiency with minimal steps. But now these needs are driven by convenience and lifestyle enhancement. Feedback also needs to be considered differently, and should strive to incentivize patients to remain adherent in order to maintain control of their disease, and where possible – improve their condition.
Attitudinal Archetypes of Chronic Disease Management
To better understand patient needs along the identified stages of their journey, we took a deeper dive within each individual stage of the Patient Journey through a study we completed with West Pharmaceutical Services. This study reveals an added layer of complexity for pharmaceutical manufacturers to take development queues from that can be invaluable in ensuring that devices as well as training, onboarding, and longitudinal adherence companion software applications are developed to support personalization and the unique needs of each patient or clinical stakeholders.
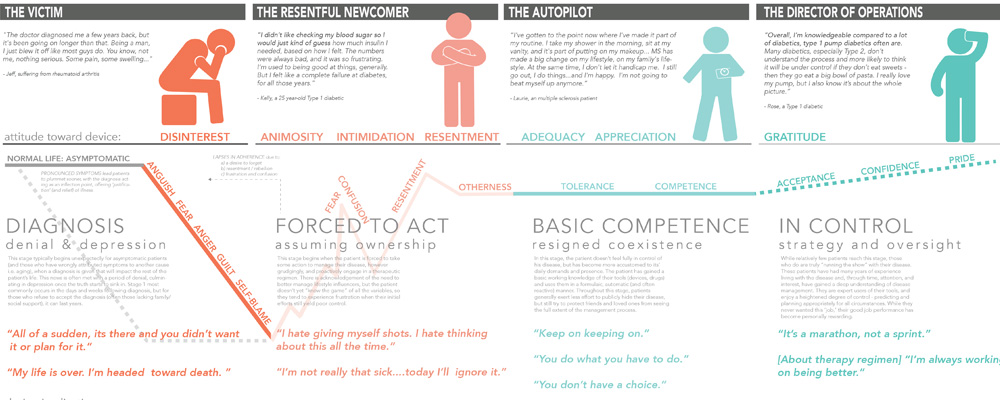
This study revealed the patient’s changing emotional and attitudinal states along their journey.
We’ve outlined the common patient trajectory that focuses on the feelings one has towards their disease and treatment and therapies. Within this trajectory, we’ve defined the four emotive stages of chronic disease within these archetypes (‘diagnosis’, ‘forced to act’, ‘basic competence’ and ‘in control’).
An understanding of both the characteristic emotional states of patients and their progression provides deep insight into patient behavior (most notably adoption drivers and barriers, and therapy adherence and deviations) that can be leveraged to facilitate both delivery device adoption and continual use.
Attitudes toward disease management (and consequently user needs) shift from that of denial and resistance to acknowledgement and acceptance within these emotive stages, and a deep understanding of the emotional drivers within each stage can help determine tangible design guidelines for each of the archetypes defined. Pharmaceutical delivery device design attributes that might support adoption and adherence vary across those stages identified. When understood by device developers – our findings can guide both emotional and physical disease management strategies.
For each of the four emotive stages identified, our research further revealed and defined the following characteristics for patients managing a chronic disease:
- Attitudinal archetypes These archetypes capture the prevailing attitudes that patients assume towards their disease during each of the unique phases. The attitudinal archetypes are distinct and relatable patient typologies that in turn influence disparate disease management modalities.
- Emotional context This context provides an understanding of the raw emotions felt by patients throughout the journey, and aims to illustrate how and why these emotions change or evolve over time.
- Relationship with treatment and device Here we examined patient attitudes toward their treatment device (syringe, autoinjector, infusion pump, etc.), and how these attitudes might influence usage. Such attitudes were drawn from analogous everyday relationships (often non-medical in nature) experienced by patients.
- Motivations to move Our findings here cite specific emotive, cognitive, and environmental shifts that might encourage or cause a patient to transition from one stage to the next.
The Big Lesson
By recognizing the distinct stages of the patient journey and the evolving physical and emotional needs therein, we are better equipped to design and develop safe, reliable, and desirable solutions that address all definitions of usability for all the types of patient that one patient might be. This foundational knowledge is applicable to all the elements of a successful chronic disease state management offering including devices (novel or platform), instructions for use, training and onboarding programs, and longitudinal adherence focused companion software and other digital health experiences. This foundation should be put in place at the onset of development activities to ensure each element of the offering is best supporting the desired clinical outcomes for the patient and health system.
To receive a full size hi-resolution poster of either The Patient Journey or Attitudinal Archetypes of Chronic Disease Management, or to learn more on this topic, please fill out the form below.

